Odontogenic onset mucormycosis in a post-COVID-19 diabetic patient: an unusual report
DOI:
https://doi.org/10.5327/2525-5711.269Palavras-chave:
Mucormycosis, Diabetes mellitus, COVID-19, Tooth abscessResumo
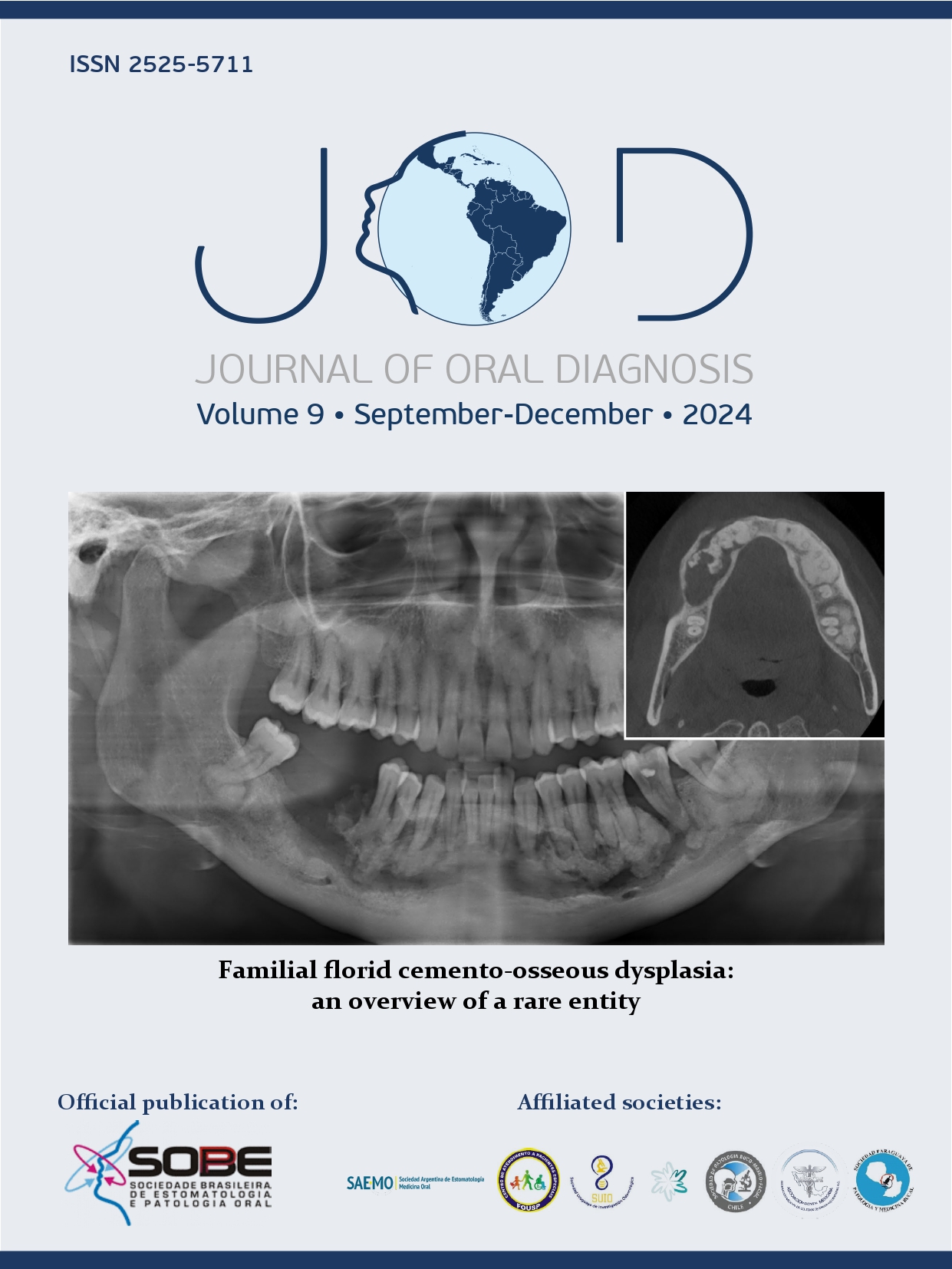
Fungal infections associated with COVID-19 have been responsible for exacerbating the course of the disease, with mucormycosis being one of the main reported conditions. Although dental involvement is commonly considered an extension of rhinocerebral disease, some authors recognize it as a distinct clinical entity characterized by odontogenic onset mucormycosis. The aim of this study was to report the diagnosis of mucormycosis following drainage of odontogenic abscess in a post-COVID-19 diabetic patient. A 69-year-old post-COVID-19 diabetic man sought a maxillofacial surgery service due to complaints of pain and swelling on the right side of the face. Edema, dental mobility, and purulent discharge associated with teeth 16 and 17 were noted. Drainage of the odontogenic abscess was performed, and cone-beam computed tomography was requested. Tomographic findings included a suggestive image of osteolytic lesion in the posterior region of the maxilla extending into the right maxillary sinus. Extraction of teeth 16 and 17 and biopsy of areas of necrotic bone were performed. Histopathological aspects favored the diagnosis of mucormycosis. The patient was referred for treatment with Amphotericin B. The diagnosis of mucormycosis should be considered in immunosuppressed patients, especially those with diabetes mellitus and post-COVID-19, presenting signs and symptoms of odontogenic infection.
Referências
World Health Organization. Coronavirus disease (COVID-19)
epidemiological updates and monthly operational updates
[Internet]. Geneva: World Health Organization, 2024 [accessed
in July 20, 2024]. Available from: https://www.who.int/
emergencies/diseases/novel-coronavirus-2019/situationreports
Naveen KV, Saravanakumar K, Sathiyaseelan A, MubarakAli
D, Wang MH. Human fungal infection, immune response, and
clinical challenge-a perspective during COVID-19 pandemic.
Appl Biochem Biotechnol. 2022;194:4244-57. https://doi.
org/10.1007/s12010-022-03979-5
Tayabali K, Pothiwalla H, Narayanan S. Epidemiology of
COVID-19-associated mucormycosis. Curr Fungal Infect Rep.
:1-20. https://doi.org/10.1007/s12281-023-00464-2
Dwivedi S, Choudhary P, Gupta A, Singh S. The cross-talk
between mucormycosis, steroids and diabetes mellitus
amidst the global contagion of COVID-19. Crit Rev
Microbiol. 2023;49(3):318-33. https://doi.org/10.1080/10408
X.2022.2052795 .
John TM, Jacob CN, Kontoyiannis DP. When uncontrolled
diabetes mellitus and severe covid-19 converge: the perfect
storm for mucormycosis. J Fungi (Basel). 2021;7(4):298.
https://doi.org/10.3390/jof7040298
Sengupta I, Nayak T. Coincidence or reality behind
Mucormycosis, diabetes mellitus and Covid-19 association: a
systematic review. J Mycol Med. 2022;32(3):101257. https://
doi.org/10.1016/j.mycmed.2022.101257
Janjua OS, Shaikh MS, Fareed MA, Qureshi SM, Khan MI,
Hashem D, et al. Dental and Oral Manifestations of COVID-19
related mucormycosis: diagnoses, management strategies
and outcomes. J Fungi (Basel). 2021;8(1):44. https://doi.
org/10.3390/jof8010044
Manesh A, Devasagayam E, Sahu S, Bhanuprasad K, Mannam
P, Karthik R, et al. Primary odontogenic onset invasive
mucormycosis-an under recognized clinical entity. Clin
Microbiol Infect. 2023;29(8):1086.e1-1086.e5. https://doi.
org/10.1016/j.cmi.2023.05.002
Saidha PK, Kapoor S, Das P, Gupta A, Kakkar V, Kumar A,
et al. Mucormycosis of paranasal sinuses of odontogenic origin
post COVID19 infection: a case series. Indian J Otolaryngol
Head Neck Surg. 2022;74(Suppl 2):3437-41. https://doi.
org/10.1007/s12070-021-02638-1
Gupta I, Baranwal P, Singh G, Gupta V. Murcomycosis, past
and present: a comprehensive review. Future Microbiol.
;18:217-34. https://doi.org/10.2217/fmb-2022-0141
Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ,
Kontoyaiannis DP. Epidemiology and clinical manifestations
of murcomycosis. Clin Infect Dis. 2012;54 Suppl 1:S23-34.
https://doi.org/10.1093/cid/cir866
Ozbek L, Topçu U, Many M, Esen BH, Bektas SN, Aydin
S, et al. COVID-19-associated murcomycosis: a systematic
review and meta-analysis of 958 cases. Clin Microbiol Infect.
;29(6):722-31. https://doi.org/10.1016/j.cmi.2023.03.008
Centers for Disease Control and Prevention. Fungal diseases
and COVID-19 [Internet]. 2020 [accessed in June 15, 2024].
Available from: https://www.cdc.gov/fungal/hcp/covid-fungal/
index.html#:~:text=COVID%2D19%20likely%20increases%20
the,the%20body’s%20defenses%20against%20fungi.
Hoenigl M., Seidel D, Sprute R, Cunha C, Oliverio M,
Goldman GH, et al. COVID-19-associated fungal infections.
Nat Microbiol. 2022;7(8):1127-40. https://doi.org/10.1038/
s41564-022-01172-2
Salazar F, Bignell E, Brown GD, Cook PC, Warris A.
Pathogenesis of respiratory viral and fungal coinfections. Clin
Microbiol Rev. 2022;35(1):e0009421. https://doi.org/10.1128/
CMR.00094-21
Heshmati HM. Interactions between COVID-19 infection and
diabetes. Front Endocrinol (Lausanne). 2024;14:1306290.
https://doi.org/10.3389/fendo.2023.1306290
Singh AK, Singh R, Joshi SR, Misra A. Mucormycosis in
COVID-19: a systematic review of cases reported worldwide
and in India. Diabetes Metab Syndr. 2021;15(4):e102146.
https://doi.org/10.1016/j.dsx.2021.05.019
Sun L, Yang X, Cao B, Su X, Wang J, Xu C. Retrospective
study of the impact of diabetes on the severity and prognosis
of COVID-19. Exp Ther Med. 2024;27(5):194. https://doi.
org/10.3892/etm.2024.12482
Mora-Martinez A, Murcia L, Rodríguez-Lozano FJ. Oral
manifestations of mucormycosis: a systemic review. J Fungi
(Basel). 2023;9(9):935. https://doi.org/10.3390/joe9090935
Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SCA,
Dannaoui E, Hochhegger B, et al. Global guideline for the
diagnosis and management of murcomycosis: an initiative
of the European Confederation of Medical Mycology in
cooperation with the Mycoses Study Group Education and
Research Consortium. Lancet Infect Dis. 2019;19(12):e405-e421.
Downloads
Publicado
Como Citar
Edição
Seção
Licença
Copyright (c) 2024 Marcelo Santos Bahia, Yuri de Lima Medeiros, Maria Emília Mota, Marcella Yumi Kadooka, Pablo Agustin Vargas, Cassio Edvard Sverzut, Alexandre Elias Trivellato

Este trabalho está licenciado sob uma licença Creative Commons Attribution 4.0 International License.