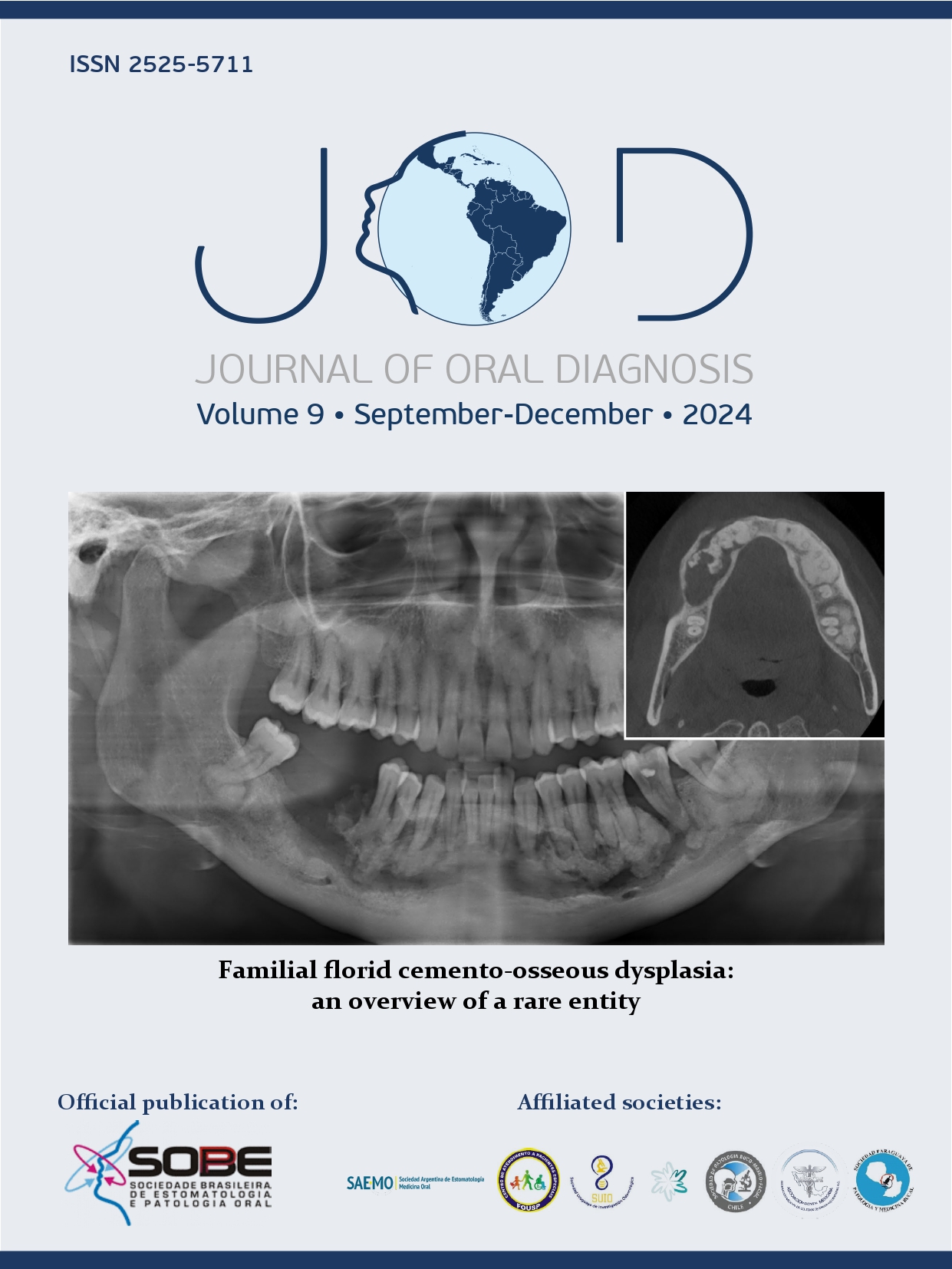
Diagnosis of HPV-associated oropharyngeal squamous cell carcinoma in a middle-income country: report of two new cases
DOI:
https://doi.org/10.5327/2525-5711.260Keywords:
HPV-associated squamous cell carcinoma, Oropharynx, Uvula, Immunohistochemistry, In situ hybridizationAbstract
Human papillomavirus (HPV)-associated oropharyngeal squamous cell carcinoma (OPSCC) is a distinct subset characterized by better treatment responses and higher survival rates. Clinical and morphological aspects are crucial for diagnosis. Here we report two additional cases of HPV-associated OPSCC. Case 1: A 46-year-old male smoker and alcoholic presented with a 6 cm asymptomatic destructive ulcer involving multiple areas of the oropharynx. Microscopic analysis revealed non-keratinizing squamous cell carcinoma (SCC) with strong and diffuse cytoplasmatic and nuclear positivity for p16 in the tumor cells on IHC and ISH for HPV16/18 revealed the presence of viral DNA in a dot-like pattern. Case 2: A 53-year-old male smoker and alcoholic complained of dysphagia and exhibited erythematous areas in the uvula. Microscopically, a basaloid SCC was observed. Assessment of p16 expression showed diffuse moderate nuclear and cytoplasmatic positivity and ISH for DNA HPV16/18 also demonstrated dot-like signals. The present cases highlight the clinical and microscopical aspects of HPV-associated OPSCC. Pathologists and clinicians must remain vigilant in identifying HPV-associated OPSCC, even in cases where there is a history of alcohol and tobacco consumption. Assessment of p16 immunohistochemical patterns and ISH analysis are crucial to better understand the scenario of HPV-associated OPSCC in middle-income countries.
References
Berman TA, Schiller JT. Human papillomavirus in cervical cancer and oropharyngeal cancer: one cause, two diseases. Cancer. 2017;123(12):2219-29. https://doi.org/10.1002/cncr.30588
Kreimer AR, Chaturvedi AK, Alemany L, Anantharaman D, Bray F, Carrington M, et al. P. Summary from an international cancer seminar focused on human papillomavirus (HPV)-positive oropharynx cancer, convened by scientists at IARC and NCI. Oral Oncol. 2020;108:104736. https://doi.org/10.1016/j.oraloncology.2020.104736
Gillison ML, Koch WM, Capone RB, Spafford M, Westra WH, Wu L, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst. 2000;92(9):709-20. https://doi.org/10.1093/jnci/92.9.709
Louredo BVR, Prado-Ribeiro AC, Brandão TB, Epstein JB, Migliorati CA, Piña AR, et al. State-of-the-science concepts of HPV-related oropharyngeal squamous cell carcinoma: a comprehensive review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2022;134(2):190-205. https://doi.org/10.1016/j.oooo.2022.03.016
El-Mofty SK, Patil S. Human papillomavirus (HPV)-related oropharyngeal nonkeratinizing squamous cell carcinoma: characterization of a distinct phenotype. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(3):339-45. https://doi.org/10.1016/j.tripleo.2005.08.001
Warnakulasuriya S, Greenspan JS. Textbook of oral cancer: prevention. diagnosis and management. New York: Springer; 2020.
Buexm LA, Soares-Lima SC, Brennan P, Fernandes PV, Lopes MSA, Carvalho FN, et al. HPV impact on oropharyngeal cancer patients treated at the largest cancer center from Brazil. Cancer Lett. 2020;477:70-5. https://doi.org/10.1016/j.canlet.2020.02.023
Elhalawani H, Mohamed ASR, Elgohari B, Lin TA, Sikora AG, Lai SY, et al. Tobacco exposure as a major modifier of oncologic outcomes in human papillomavirus (HPV) associated oropharyngeal squamous cell carcinoma. BMC Cancer. 2020;23;20(1):912. https://doi.org/10.1186/s12885-020-07427-7
Lewis JS Jr, Beadle B, Bishop JA, Chernock RD, Colasacco C, Lacchetti C, et al. Human papillomavirus testing in head and neck carcinomas guideline from the College of American Pathologists. Arch Pathol Lab Med. 2018;142(5):559-97. https://doi.org/10.5858/arpa.2017-0286-CP
Fakhry C, Lacchetti C, Rooper LM, Jordan RC, Rischin D, Sturgis EM, et al. Human papillomavirus testing in head and neck carcinomas: ASCO clinical practice guideline endorsement of the College of American Pathologists Guideline. J Clin Oncol. 2018;36(31):3152-61. https://doi.org/10.1200/JCO.18.00684
Overton LJ, Fritsch VA, Lentsch EJ. Squamous cell carcinoma of the uvula: an analysis of factors affecting survival. Laryngoscope. 2013;123(4):898-903. https://doi.org/10.1002/lary.23648
Okami K. Clinical features and treatment strategy for HPV‐related oropharyngeal cancer. Int J Clin Oncol. 2016;21(5):827-35. https://doi.org/10.1007/s10147-016-1009-6
Safaeian M, Porras C, Schiffman M, Rodriguez AC, Wacholder S, Gonzalez P, et al. Epidemiological study of anti-HPV16/18 seropositivity and subsequent risk of HPV16 and -18 infections. J Natl Cancer Inst. 2010;102(21):1653-62. https://doi.org/10.1093/jnci/djq384
Lu B, Viscidi RP, Wu Y, Lee JH, Nyitray AG, Villa LL, et al. Prevalent serum antibody is not a marker of immune protection against acquisition of oncogenic HPV16 in men. Cancer Res. 2012;72(3):676-85. https://doi.org/10.1158/0008-5472.CAN-11-0751
Drake VE, Fakhry C, Windon MJ, Stewart CM, Akst L, Hillel A, et al. Timing, number, and type of sexual partners associated with risk of oropharyngeal cancer. Cancer. 2021;127(7):1029-38. https://doi.org/10.1002/cncr.33346
Ferris RL, Flamand Y, Weinstein GS, Li S, Quon H, Mehra R, et al. Phase II randomized trial of transoral surgery and low-dose intensity modulated radiation therapy in resectable p16+ locally advanced oropharynx cancer: an ECOG-ACRIN Cancer Research Group Trial (E3311). J Clin Oncol. 2022;40(2):138-49. https://doi.org/10.1200/JCO.21.01752
Parvathaneni U, Lavertu P, Gibson M, Glastonbury CM. Advances in diagnosis and multidisciplinary management of oropharyngeal squamous cell carcinoma: state of the art. Radiographics. 2019;39(7):2055-68. https://doi.org/10.1148/rg.2019190007
van Gysen K, Stevens M, Guo L, Jayamanne D, Veivers D, Wignall A, et al. Validation of the 8th edition UICC/AJCC TNM staging system for HPV associated oropharyngeal cancer patients managed with contemporary chemo-radiotherapy. BMC Cancer. 2019;19(1):674. https://doi.org/10.1186/s12885-019-5894-8
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tân PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24-35. https://doi.org/10.1056/NEJMoa0912217
De Cicco R, Menezes RM, Nicolau UR, Pinto CAL, Villa LL, Kowalski LP. Impact of human papillomavirus status on survival and recurrence in a geographic region with a low prevalence of HPV-related cancer: a retrospective cohort study. Head Neck. 2020;42(1):93-102. https://doi.org/10.1002/hed.25985
Louredo BVR, Prado-Ribeiro AC, Brandão TB, Epstein JB, Migliorati CA, Piña AR, et al. State-of-the-science concepts of HPV-related oropharyngeal squamous cell carcinoma: a comprehensive review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2022;134(2):190-205. https://doi.org/10.1016/j.oooo.2022.03.016
Chaturvedi AK, Anderson WF, Lortet-Tieulent J, Curado MP, Ferlay J, Franceschi S, et al. Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers. J Clin Oncol. 2013;31(36):4550-9. https://doi.org/10.1200/JCO.2013.50.3870
Mariz BALA, Kowalski LP, William Jr. WN, Castro Jr G, Chaves ALF, Santos M, et al. Global prevalence of human papillomavirus-driven oropharyngeal squamous cell carcinoma following the ASCO guidelines: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2020;156:103116. https://doi.org/10.1016/j.critrevonc.2020.103116
Barauna Neto JC, Barauna MR, Aota KG. Epidemiological profile of oropharynx cancer in Brazil from 2013 to 2022. Arch Head Neck Surg. 2024;53:e20240001. https://doi.org/10.4322/ahns.2024.0001
Carvalho RS, Scapulatempo-Neto C, Curado MP, Capuzzo RC, Teixeira FM, Pires RC, et al. HPV-induced oropharyngeal squamous cell carcinomas in Brazil: prevalence, trend, clinical, and epidemiologic characterization. Cancer Epidemiol Biomarkers Prev. 2021;30(9):1697-707. https://doi.org/10.1158/1055-9965.EPI-21-0016
Pires RC, Carvalho R, Gama RR, Carvalho AL, Santos CR, Capuzzo RC. Progressive increase trend in HPV-related oropharyngeal squamous cell carcinoma in Brazil. Int Arch Otorhinolaryngol. 2021;26(1):e132-e136. https://doi.org/10.1055/s-0041-1730297
Anantharaman D, Abedi-Ardekani B, Beachler DC, Gheit T, Olshan AF, Wisniewski K, et al. Geographic heterogeneity in the prevalence of human papillomavirus in head and neck cancer. Int J Cancer. 2017;140(9):1968-75. https://doi.org/10.1002/ijc.30608
Instituto Nacional de Câncer José Alencar Gomes da Silva. Estimativa 2020: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2022.
Louredo BVR, Curado MP, Penafort PVM, Arruda JAA, Abreu LG, Mesquita RA, et al. Contribution of public oral pathology services to the diagnosis of oral and oropharyngeal cancer in Brazil. Braz Oral Res. 2023;37:e126. https://doi.org/10.1590/1807-3107bor-2023.vol37.0126
Abrahão R, Perdomo S, Pinto LFR, Carvalho FN, Dias FL, Podestá JRV, et al. Predictors of survival after head and neck squamous cell carcinoma in South America: the InterCHANGE study. JCO Glob Oncol. 2020;6:486-99. https://doi.org/10.1200/GO.20.00014
Louredo BV, Vargas PA, Pérez-de-Oliveira ME, Lopes MA, Kowalski LP, Curado MP. Epidemiology and survival outcomes of lip, oral cavity, and oropharyngeal squamous cell carcinoma in a southeast Brazilian population. Med Oral Patol Oral Cir Bucal. 2022;27(3):e274-e284. https://doi.org/10.4317/medoral.25147
Costa AAS, Caldeira PC, Sousa AA, Tibúrcio JD, Belligoli LQG, Santos VB, et al. Oral and oropharyngeal cancer: time from first symptoms to treatment initiation and associated factors. Braz Oral Res. 2023;37:e054. https://doi.org/10.1590/1807-3107bor-2023.vol37.0054
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Sibele Nascimento de Aquino, Hélen Kaline Farias Bezerra, Brendo Vinícius Rodrigues Louredo, Márcio Ajudarte Lopes, Alan Roger Santos-Silva, Pablo Agustin Vargas

This work is licensed under a Creative Commons Attribution 4.0 International License.